UTSW Hackathon 2019
On November 8-10th, I was able to compete in The University of Texas Southwestern Medical School U-Hack Med Hackathon. I attended the event last year and helped multiple groups as a facilitator and mentor, but this year I applied to compete on a team and was accepted! The 48-hour event was a great learning experience and an amazing way to meet new people from varied backgrounds.
I was on Team 9. Our team’s project was entitled “REAL-TIME CARDIAC ASSESSMENT OF CATHETERIZATION-DERIVED FICK AND CMR-DERIVED FLOW” and focused on using machine learning and AI to reduce the time it takes for children to undergo pediatric heart catherization procedures. For a full description of the project, click here. In the procedure, a wire with a balloon attached to the end is inserted into a large vein near the child’s groin, then guided up through the torso into the heart and surrounding veins and arteries. In the past, this procedure has been done using x-rays to allow the physician to see the wire as it moves. However, this makes an already risky procedure even more dangerous. Studies have shown that children that are exposed to 2-4 hours of x-rays (the amount of time a procedure typically takes) are 3-4 times more likely to develop cancer later in life. More recently, cardiologists have been performing radiation-free heart catheterizations using an MRI to view the wire and balloon. In both procedures, the child has to be put under general anesthesia for the entire time. This much anesthesia carries a high risk of causing developmental and neurological problems. Thus, anything that can be done to reduce the exposure to x-rays and amount of time the child is under anesthesia can significantly reduce potential risks. This was our challenge. Click here for more info on radiation-free heart catheterizations at Children’s Medical Center in Dallas.
Dr. Youssef Arar, a pediatric cardiology fellow at Children’s Medical Center in Dallas was our team lead. Dr. Daniel Castellanos, a pediatric cardiology fellow and colleague of Dr. Arar, was our co-lead. they routinely perform these procedures so they are well acquainted with the intricacies, risks, and ways the procedures can possibly be improved. Dr. Arar presented us with two different tasks that could help reduce the time heart cath procedures take.
The first challenge involved automating calculations of blood flow and pressures. Currently, the physician doing the procedure has to tell a technician what values he is getting. The technician then enters those values into a spreadsheet and has to manually calculate the blood flow and pressure. This is a time consuming and error prone process. Every moment calculations are being performed manually is another moment the child is exposed to radiation or under anesthesia. When the procedure is done in the MRI room, there is a tremendous amount of noise, so communication is impaired significantly. This makes the process even more error prone. Our team developed a web-based application to automate the calculations. To use the app, the values are relayed to the technician, or the technician views them on a screen. As they are input, blood flow, pressure, and other values are automatically calculated, giving the physician immediate answers. Dr. Arar said this app could potentially shorten procedures by 40 minutes and give more accurate calculations!
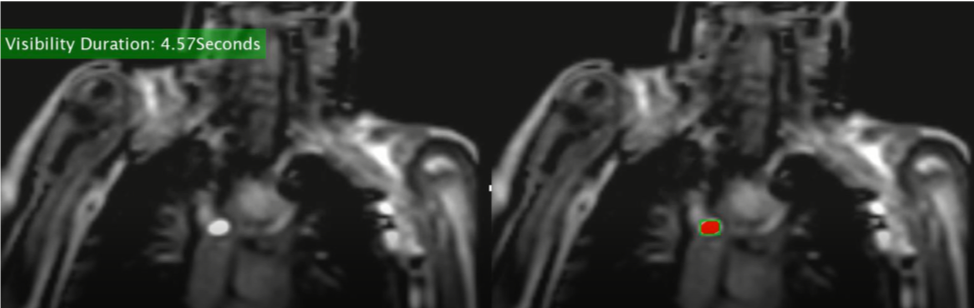
The second challenge involved visualizing the balloon in the heart during the MRI procedure. An MRI takes an image of a single plane at any given time. If the balloon is not in that plane, the cardiologist cannot see it, so any movement of the balloon is done blindly. This results in the patient having to potentially be repositioned, lengthening the anesthesia time. Dr. Arar asked us to find a way to track the amount of time the balloon is seen during a procedure. By knowing this information, the cardiologists can evaluate the procedure after it is finished to discuss what could have been done differently to keep the balloon in view longer. By determining what adjustments can be made, future procedures can be more efficient, shorter, and safer. Our team used a process called “thresholding” to segment the balloon on the MRI image and count the number of frames it appeared in. This allowed us to calculate the percentage of time the balloon was seen.
Overall, I had a fantastic time. My team was small and we had varied backgrounds. We had a web developer, a computational scientist, a post-doctoral researcher, a PhD student, two MDs, and myself. In the end, our team ended up winning the Lyda Hill Best Overall Team award for our work. Great job everyone!
Team Members:
- Dr. Yousef Arar, MD, Pediatric Cardiology Fellow, Children’s Medical Center Dallas – Team Lead
- Dr. Daniel Castellanos, MD, Pediatric Cardiology Fellow, Children’s Medical Center Dallas – Team Co-Lead
- Anupam Kumar, PhD Student, Vanderbilt University
- Krishna Kanth Chitta, Computational Scientist, UT Southwestern Medical Center
- Lokesh Basavarajappa, Post-doctoral researchers, University of Texas at Dallas
- Yasasvini Puligundla, Web developer, Parkland Center for Clinical Innovation
- John Pace, Sr. Data Scientist, Mark III Systems